Table of Contents
ToggleEgg freezing offers a way to hit “pause” on your biological clock. It lets you focus on your career, personal goals, or whatever is important. But what makes egg freezing more or less successful?
Studies1 show that for about 18% of women, especially as they get older, egg freezing doesn’t work. Hormones and egg counts are significant factors for this. Imagine starting life with a million eggs, only to lose a thousand each month. The rate even speeds up after age 35.2
This blog will break down why your egg count and hormone levels matter. Let’s dive in.
What Is the Success Rate of Egg Freezing?
Let’s start with the big question: How often does egg freezing work?
Success here means two things: pregnancies and live births from frozen eggs.
Generally, about 85 of 100 eggs survive after freezing1 and then thawing. Of these, 67 become pregnancies.3
The most critical part is that about 34 of 100 eggs result in live births.
What Factors Contribute to Egg Freezing Success?
So, what can you do to maximize your successful egg-freezing chances?
Several factors come into play:
- Age: This is the big one. As you get older, you have fewer good eggs. Less good eggs mean less chance of success.
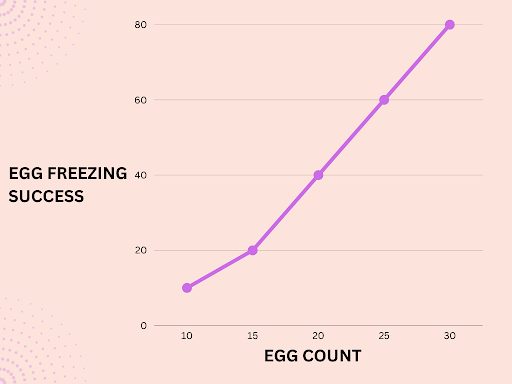
- Number of Eggs: You need about 15 to 20 eggs for the best odds.4 With that many, you have a 70% chance of having a baby.
- Freezing Method: The egg-freezing method matters. For example, a quick freeze method called vitrification works well, with a 94.5% success rate.5
- Health Conditions: Issues like PCOS or metabolic disorders can lower your odds. Bad habits like smoking can, too.
- Clinic Skill: How good the clinic is at hormone treatment and egg freezing also counts.
Impact of Egg Count on Egg Freezing: How Does Egg Count Affect Egg Freezing Success?
The more mature, high-quality eggs you can freeze, the better your chances of live birth later.
Here’s a breakdown of the ideal egg count for each age group:
- If you’re 35 or younger, aim for 14 mature eggs. With that, you have an 80% chance of a live birth later.6
- Between 35 and 37? You’ll need at least 15 eggs for a 70% chance.7
- Aged 38 to 40? Aim for 16 eggs.
- Between 41 and 42? The number jumps to 28.
- Over 42? You’d need a whopping 80 mature eggs.
What Is Ovarian Reserve and Why Does it Matter?
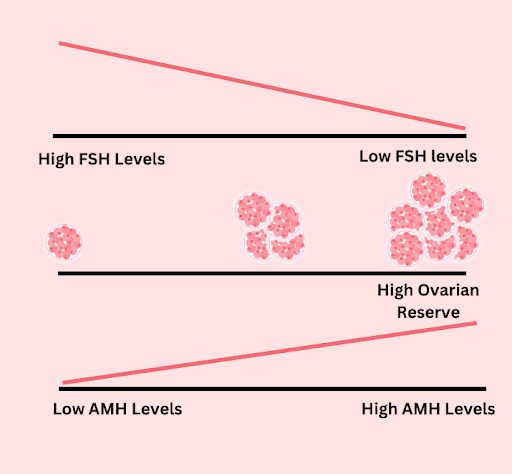
Ovarian reserve8 is a count of how many good eggs you have left. It helps doctors figure out your chances of having a baby.
A high ovarian reserve is a good sign of egg-freezing success. The more good eggs you have, the better your chances of a successful pregnancy later.
How is Ovarian Reserve Measured?
The following tests can provide a measure of your ovarian reserve:
- FSH (Follicle-Stimulating Hormone) and Estradiol Levels: Doctors check these on Day 3 of your period.8 High levels mean you have fewer good eggs left.
- AMH (anti-Müllerian Hormone) Levels: Low AMH means fewer eggs.9
- Antral Follicle Count (AFC): This is a picture of your ovaries. More follicles mean more good eggs.
- Clomiphene Challenge Test (CCT): This is a two-step test. First, doctors check FSH levels on Day 3 of your cycle.10 Then, you take a pill for a few days. Following this, doctors re-check FSH levels. A low level in this test refers to fewer good eggs.
How Do Hormones Affect Egg Freezing Success?
Hormones tell us a lot about your egg count. The two big ones are AMH and FSH.
AMH shows us how many eggs you have left. In one study,11 high AMH levels led to the retrieval of 60% of mature eggs. The number was only 5% with low AMH.
FSH tells us about the egg quality. Thus, low AMH and high FSH mean fewer, lower-quality eggs.12
What Are the Hormones Involved in Egg Freezing?
Three hormones are essential for egg freezing: AMH, FSH, and LH (Luteinizing Hormone).
What Is Anti-Mullerian Hormone (AMH) and Its Role in Egg Freezing?
The ovaries make AMH or anti-Mullerian hormone.13 It helps your body prepare for a baby by helping with your menstrual cycle and uterus development.
As you get older, the AMH levels fall.14 This is a sign you may have few eggs left. For example, a study15 evaluated 2,585 women who had trouble getting pregnant. The study found that these women had low AMH levels and egg count.
Importance of Follicle-Stimulating Hormone (FSH) in Egg Freezing
FSH, or Follicle-Stimulating Hormone,16 is critical in getting your ovaries to make eggs.
This is why doctors give you extra FSH to help your body make more mature eggs.17
One study18 found that women who got extra FSH had ten eggs collected. Those who didn’t get extra FSH had only eight eggs collected. Also, the chance of getting pregnant was higher in the FSH group, at 28.2%, compared to 24.8% in the no-FSH group.
Role of Luteinizing Hormone (LH) in Egg Freezing
Luteinizing Hormone (LH)19 tells your ovaries when to release an egg.
Doctors want to avoid that from happening too soon during the egg-freezing process. They use medicines like GnRH to keep LH levels low. This helps ensure the eggs stay in the ovaries until they are mature.
Once the eggs are ready, doctors administer a hormone called “human chorionic gonadotropin” or HCG.20 This creates a fake LH surge. As a result, about 36 hours after getting this hormone, doctors can collect the mature eggs.
The method helps control the egg retrieval process, making it more likely for you to have good eggs for freezing.
Can Age and Lifestyle Affect Hormone Levels and Egg Count?
Your age and how you live your life affect your egg count and hormone levels. This, in turn, can influence your egg-freezing success.
How Does Age Affect Egg Count and Hormone Levels?
Age isn’t just a number for egg freezing. 80% of women freeze their eggs in their late 30s. But at that age, you often have fewer good eggs.
This is because AMH levels drop by 6% as women age.21 The result is a 4.5% decrease in ready-to-grow follicles (the precursors to mature eggs).
In other words, if you’re over 35, you’re 97.1% less likely to get more than three mature eggs22 than women under 35.
How do Lifestyle Factors Affect Egg Count and Hormone Levels?
- Impact of Diet
Your food choices are critical. One study23 showed that women with high fat and alcohol intake had low fertility rates. This is because a diet high in fat and sugar messes the way eggs grow. A balanced diet is best for your egg count and hormone levels.
- Smoking
Smoking can lower your egg count24 by lowering AMH levels and raising FSH.
- Stress
Stress can stop you from ovulating.25 When you’re stressed, your body makes a hormone called cortisol. This hormone can block other hormones that help you ovulate. So, less stress means a better chance of freezing your eggs.
Takeaway
In a nutshell, egg freezing is a powerful option for women who want to keep the door open for pregnancy later in life. But success isn’t guaranteed. Your age, the number of eggs you have, and lifestyle choices can all make a big difference.
Hormones like AMH and FSH can provide clues about the quantity and quality of your eggs. So, before you leap, ensure you get the complete picture of your fertility health.
Sources
- Walker Z, Lanes A, Ginsburg E. Oocyte cryopreservation review: outcomes of medical oocyte cryopreservation and planned oocyte cryopreservation. Reprod Biol Endocrinol. 2022;20. doi:10.1186/s12958-021-00884-0
- Esteves SC, Yarali H, Vuong LN, Carvalho JF, Özbek İY, Polat M, et al. Antral follicle count and anti-Müllerian hormone to classify low-prognosis women under the POSEIDON criteria: a classification agreement study of over 9000 patients. Hum Reprod. 2021;36(6). doi:10.1093/humrep/deab056
- Kakkar P, Geary J, Stockburger T, Kaffel A, Kopeika J, El-Toukhy T. Outcomes of Social Egg Freezing: A Cohort Study and a Comprehensive Literature Review. J Clin Med Res. 2023;12(13). doi:10.3390/jcm12134182
- Mizrachi Y, Horowitz E, Farhi J, Raziel A, Weissman A. Ovarian stimulation for freeze-all IVF cycles: a systematic review. Hum Reprod Update. 2020;26(1). doi:10.1093/humupd/dmz037
- Pujol A, Zamora MJ, Obradors A, Garcia D, Rodriguez A, Vassena R. Comparison of two different oocyte vitrification methods: a prospective, paired study on the same genetic background and stimulation protocol. Hum Reprod. 2019;34(6). doi:10.1093/humrep/dez045
- Gale J, Clancy AA, Claman P. Elective egg freezing for age-related fertility decline. CMAJ. 2020;192(6):E142.
- New Extend Fertility research analyzes estimated success rates after 1 or 2 cycles of egg freezing. Extend Fertility. Published July 1, 2020. https://extendfertility.com/extend-fertility-research-egg-freezing-success-rates-one-cycle/. Accessed September 15, 2023
- Ulrich ND, Marsh EE. Ovarian Reserve Testing: A Review of the Options, Their Applications, and Their Limitations. Clin Obstet Gynecol. 2019;62(2). doi:10.1097/GRF.0000000000000445
- Liu XY, Yang YJ, Tang CL, Wang K, Chen JJ, Teng XM, et al. Elevation of antimüllerian hormone in women with polycystic ovary syndrome undergoing assisted reproduction: effect of insulin. Fertil Steril. 2019;111(1). doi:10.1016/j.fertnstert.2018.09.022
- Deadmond A, Koch CA, Preston Parry J. Ovarian Reserve Testing. In: Endotext [Internet]. MDText.com, Inc.; 2022.
- Umarsingh S, Adam JK, Krishna SBN. The relationship between anti-Müllerian hormone (AMH) levels and pregnancy outcomes in patients undergoing assisted reproductive techniques (ART). PeerJ. 2020;8. doi:10.7717/peerj.10390
- Jain M, Singh M. Assisted Reproductive Technology (ART) Techniques. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- di Clemente N, Racine C, Pierre A, Taieb J. Anti-Müllerian Hormone in Female Reproduction. Endocr Rev. 2021;42(6). doi:10.1210/endrev/bnab012
- Moolhuijsen LME, Visser JA. Anti-Müllerian Hormone and Ovarian Reserve: Update on Assessing Ovarian Function. J Clin Endocrinol Metab. 2020;105(11):3361.
- Sun X, Xiong W, Liu L, Xiong J, Liao C, Lan Y, et al. Comparison of the predictive capability of antral follicle count vs. the anti-Müllerian hormone for ovarian response in infertile women. Front Endocrinol . 2022;13. doi:10.3389/fendo.2022.862733
- Orlowski M, Sarao MS. Physiology, Follicle Stimulating Hormone. In: StatPearls [Internet]. StatPearls Publishing; 2023.
- Ye M, Yeh J, Kosteria I, Li L. Progress in Fertility Preservation Strategies in Turner Syndrome. Frontiers in Medicine. 2020;7. doi:10.3389/fmed.2020.00003
- Vignarajan CP, Singh N, Vanamail P. The Effect of Follicle-Stimulating Hormone Administration on the Day of Human Chorionic Gonadotropin Trigger on Assisted Reproductive Technique Outcomes in Patients Undergoing In vitro Fertilization-Embryo Transfer: A Retrospective Cohort Study. J Hum Reprod Sci. 2020;13(3):196.
- Nedresky D, Singh G. Physiology, Luteinizing Hormone. In: StatPearls [Internet]. StatPearls Publishing; 2022.
- Deng L, Chen X, Blockeel C, Ye DS, Chen SL. Intramuscular injection of human chorionic gonadotropin prior to secretory transformation in patients undergoing frozen-thawed embryo transfer cycles. Reprod Biol Endocrinol. 2020;18(1). doi:10.1186/s12958-020-00606-y
- Khan HL, Bhatti S, Suhail S, Gul R, Awais A, Hamayun H, et al. Antral follicle count (AFC) and serum anti-Müllerian hormone (AMH) are the predictors of natural fecundability have similar trends irrespective of fertility status and menstrual characteristics among fertile and infertile women below the age of 40 years. Reprod Biol Endocrinol. 2019;17(1). doi:10.1186/s12958-019-0464-0
- Hosseinzadeh F, Kabodmehri R, Mehrafza M, Mansour-Ghanaei M, Sorouri ZZ, Gashti NG, et al. The Effect of Age and AMH Level on ART Outcomes in Patients With Reduced Ovarian Reserve: A Retrospective Cross-Sectional Study. J Obstet Gynaecol India. 2022;72(5). doi:10.1007/s13224-021-01582-y
- Emokpae MA, Brown SI. Effects of lifestyle factors on fertility: practical recommendations for modification. Reproduction & Fertility. 2021;2(1):R13.
- Konstantinidou F, Stuppia L, Gatta V. Looking Inside the World of Granulosa Cells: The Noxious Effects of Cigarette Smoke. Biomedicines. 2020;8(9). doi:10.3390/biomedicines8090309
- Silvestris E, Lovero D, Palmirotta R. Nutrition and Female Fertility: An Interdependent Correlation. Front Endocrinol . 2019;10. doi:10.3389/fendo.2019.00346
Anna Haotanto is the Founder of Zora Health and a passionate advocate for women’s empowerment. Anna’s personal experiences with egg-freezing, PCOS and the challenges of fertility have fueled her mission to provide high-quality information, financing, and support to help women and couples navigate their fertility journeys with confidence. She is also recognised for her achievements in finance, entrepreneurship, and women’s empowerment, and has been featured in various media outlets. You can also follow her on Linkedin or Instagram.