Women worldwide are embracing IVF (in-vitro fertilization). It’s more than a fertility solution. It’s a chance to overcome unique hurdles.
The numbers don’t lie. 1 in 8 US couples face infertility. Since 1978, IVF has helped birth over 5 million kids globally.
Moreover, in 2020, the IVF market stood at $4905 million. By 2027, it will likely jump to $5563 million. That’s a 6.8% increase. This growth speaks volumes.
It shows IVF’s essential role in today’s reproductive landscape. So, let’s break down its step-by-step journey. Here’s what we’ll cover:
Table of Contents
ToggleWhat is IVF, and Who is a Good Candidate for IVF Treatment?
“In-vitro fertilization” refers to growing embryos (early forms of babies) outside the body. So people can have babies even if they:
- Struggle with specific fertility issues, such as polycystic ovarian syndrome or endometriosis. Without IVF, women with these conditions may never get pregnant.
- Are worried about passing down risky genes. The IVF process includes screening for such genes.
- Are single or have a same-sex partner. The number of these couples turning to IVF has increased — from 13.4% to 56.2% in 19 years.
- Are focused on other goals and want to have children later in life.
Good IVF candidates are:
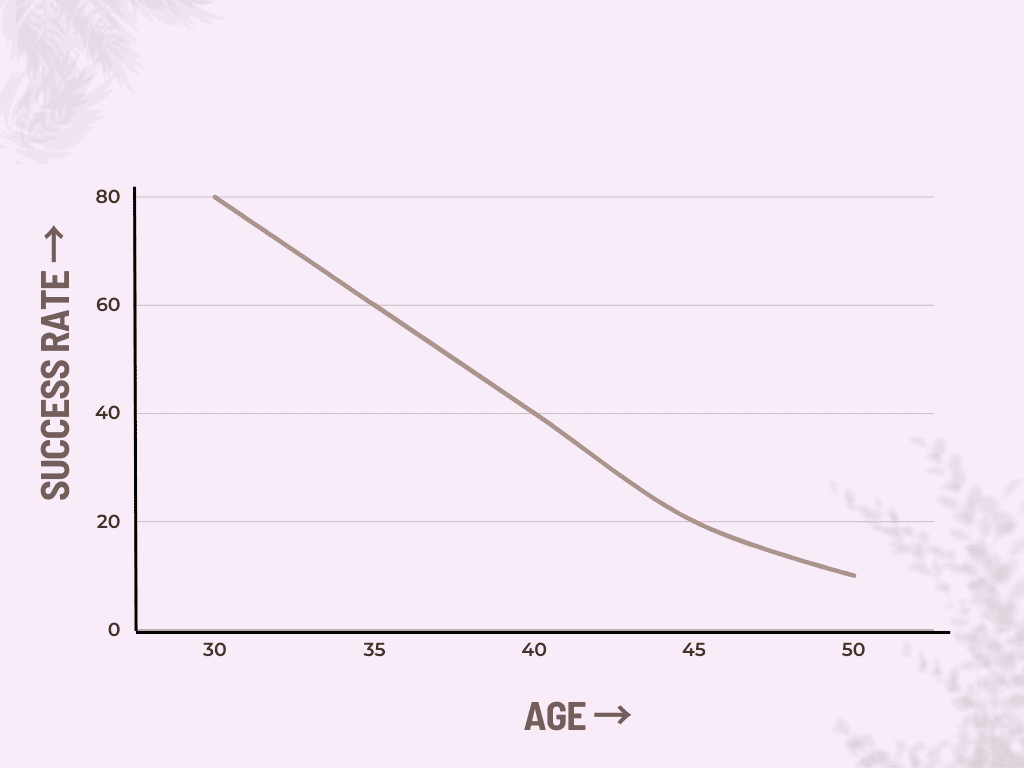
- Aged 35 or younger. Women below 30 have a 69.4% success rate with IVF. Over 40, this number drops to 13.4%.
- In good health. Conditions like diabetes lower success rates with IVF.
While these criteria can boost IVF success rates, they’re not absolute requirements. Many people who don’t fit these criteria benefit from IVF. So, if you’re considering this journey, consult a fertility specialist. This will help you understand your chances and options.
How to Prepare for the IVF Treatment Process?
- Start with a specialist chat. They will dive into your health history and discuss the IVF process. You’ll also undergo blood tests and ultrasounds.
- Lifestyle tweaks come next. Eat well and avoid smoking or alcohol. In a study, avoiding alcohol boosted oocyte retrieval by 13%. Moreover, a healthy lifestyle pushed live birth rates to 50%.
- Also, focus on your mental health. The process can be emotionally draining, which can affect success rates. Avoid stress and try yoga or meditation. A 90-minute relaxation training session can increase the IVF success rate to 76%.
- Plan your finances because IVF can be pricey. Check your insurance, too, because it often falls short. Many face poor reimbursement, leading to tough financial decisions. As a result, a significant 37.5% of couples forgo consultation. Even more concerning, 42% halt treatment due to costs.
- Optimize your schedule. Your menstrual cycle dictates IVF timing. So, date flexibility is crucial.
The Five-Stage Process of IVF: A Detailed Exploration
After understanding the preparations, let’s dissect the IVF process.
Stage 1: Ovarian Stimulation
More mature eggs lead to greater IVF success. This is because more mature eggs lead to better embryos. As a result, implantation and pregnancy chances increase.
To boost the number of mature eggs, doctors stimulate the ovaries. They do this by administering hormones like FSH (Follicle-stimulating hormone) and LH (Luteinizing hormone). These hormones act like body signals, boosting follicle growth. Each follicle houses an egg.
Doctors then track these follicles with ultrasound. They also watch your hormone levels. This allows them to determine when the eggs are ready for final maturation.
To push the eggs through this final stage, doctors give HCG (human chorionic gonadotropin).
Stage 2: Egg Retrieval
Once the eggs are mature, the next step is to retrieve them.
Doctors use a needle (under ultrasound guidance) to reach the ovaries. When the needle enters a mature follicle, it pulls the egg and its fluid into a test tube. Generally, doctors collect 10-20 mature eggs during this process.
Many factors during this stage affect the IVF success rate. These include:
- The time interval between the HCG shot and egg retrieval. Usually, a 37-hour window produces the best results.
- Use of follicular flushing. This has a 10% greater birth rate than traditional methods.
- Anesthesia type. Conscious sedation (as opposed to general anesthesia) has better success rates.
- Size of aspiration needles. Single-lumen needles with a 17/18 gauge are ideal.
- The aspiration pressure. 100-200mm of Hg is ideal.
Stage 3: In-Vitro Fertilization
The next step is to mix the collected eggs and sperm in a particular dish. Each egg receives roughly 115,000 sperm.
Doctors place this dish in an incubator, which mirrors a woman’s body. The ideal conditions are as follows:
- Air with less than 800 ppb chemical evaporates.
- A constant temperature of 37 degrees Celsius
- pH between 7.2-7.4
Soon, the eggs and sperm fuse, i.e. fertilization occurs. This leads to embryo formation. Doctors observe these embryos for 3-5 days.
They may also use advanced techniques at this stage to boost IVF success. For example, time-lapse systems boost embryo growth to 31%. This is 8% higher than with traditional methods.
Stage 4: Embryo Transfer
Next, doctors choose the embryo to transfer. The choice is between:
- Day-3 embryos, termed “cleavage,” or
- Day-5 embryos, known as “blastocysts.”
Doctors prefer blastocysts. They’ve shown a higher pregnancy rate (26%) than cleavage transfers. Plus, using blastocysts reduces the risk of multiple pregnancies.
Picking the healthiest embryo is critical to IVF success. Doctors maximize their chance of selecting the right one by:
- Transferring more than one embryo. One study highlighted a 69.9% success rate when transferring a single embryo. The success rates soared to 95.2% when using three embryos.
- Using (pre-implantation) genetic testing. Embryos that underwent this boasted a 49.5% live birth rate. Without it, the rate was 38.6%. Genetic testing allows for the selection of the best embryos. This is because it can detect congenital abnormalities. Embryos with these abnormalities either don’t develop or lead to miscarriage.
Following embryo selection, doctors assess the woman’s uterine lining. This is to ensure it’s ready for implantation.
The actual transfer involves an ultrasound-guided catheter. This tool places the chosen embryo inside the uterus, 1-2 cm below its top part. The transfer usually happens on days 18 or 19 of the menstrual cycle.
Stage 5: Luteal Phase Support
Following embryo placement, maintaining the uterus environment is crucial. This is because any uterine contractions might push the embryo out.
Luteal phase medications help here. They prevent the uterus from contracting too much. Research backs up the importance of these medications. For example, a study showed that women on progesterone medication had a 39% pregnancy rate. Without it, the rate dropped to 24.1%.
Varieties within the IVF Process: What are the Different Types of IVF Treatments?
| IVF Type | Description | Pros/Cons | Success rates |
| Conventional IVF | Retrieves multiple eggs |
|
|
| Mild IVF | Aims to retrieve a smaller number of eggs |
| Equally effective as conventional IVF |
| Natural IVF | Relies on the menstrual cycle for only one egg |
|
|
What to Expect During and After the IVF Treatment Process?
Navigating the IVF journey is intense. It’s a physical and emotional rollercoaster. Knowing what to expect allows people to cope better. This also boosts success rates.
On the physical side, expect daily injections for 8-14 days. You must visit the hospital every 2-3 days so doctors can track follicle growth. You may have to spend hours in the hospital during the egg retrieval.
The emotional challenges are even more remarkable. Outcomes are unpredictable, causing anxiety. Daily injections are taxing. The financial stress is enormous. On top of that, negative results can be hard to take.
What are the Costs of the IVF Treatment Process?
A single IVF cycle costs between 20,000-40,000 SGD ($15,000-$30,000). The cost variance is due to location, your situation and the need for extra tests or procedures.
Here’s a breakdown of IVF costs:
| Cost (SGD) | Cost (USD) | |
| Initial consultation | 130-700 | $100-$500 |
| Ovarian stimulation | 3500-7000 | $2500-$5000 |
| Egg retrieval | 1400-7000 | $1000-$5000 |
| Fertilization | 1400-4000 | $1000-$3000 |
| Embryo transfer | 1400-4000 | $1000-$3000 |
| Medications | 4000-7000+ | $3000-$5000+ |
| Miscellaneous costs | 700-2700+ | $500-$2000+ |
What are the Success Rates of the IVF Treatment Process?
IVF success rates fluctuate based on clinic expertise. This is why you’ll notice a wide range of quoted figures. For example, the NHS reports success rates between 5% and 32%.
Likewise, a study quotes live birth rates from 3.9% to 50.8%.
Thus, picking your fertility clinic is crucial to IVF success. So choose wisely.
Takeaway
IVF is a blend of science and hope. It demands courage coupled with informed choices. With each step, you’re not pursuing a procedure but a dream.
For the best chances, lean on experts and rely on evidence. Your journey to family is worth every stride. Contact us today!
Anna Haotanto is the Founder of Zora Health and a passionate advocate for women’s empowerment. Anna’s personal experiences with egg-freezing, PCOS, perimenopause and the challenges of fertility have fueled her mission to provide high-quality information, financing, and support to help women and couples navigate their fertility journeys with confidence. She is also recognised for her achievements in finance, entrepreneurship, and women’s empowerment, and has been featured in various media outlets. You can also follow her on Linkedin or Instagram.